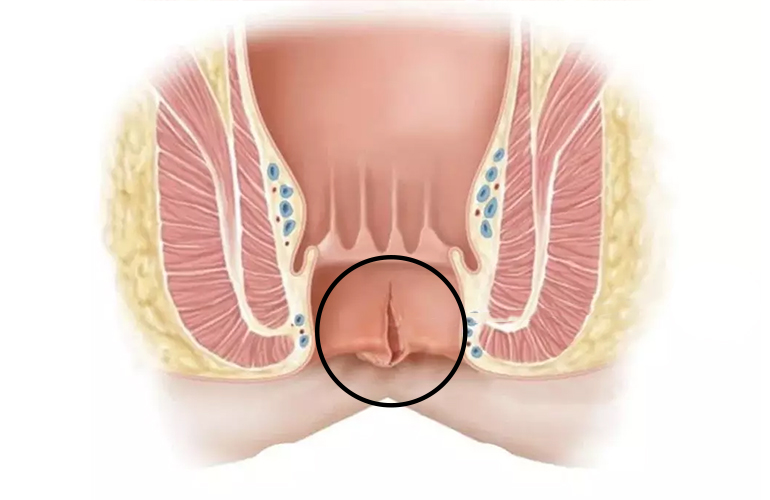
Anal Fissure
General SurgeryThese are tears that occur within the anal canal and extend to the outer skin layer, involving the intra-anal mucosa. They mostly occur during difficult straining and in the area from the mucocutaneous junction to the dentate line.
Due to the pain that occurs after the fissure is formed, defecation becomes more difficult with the reflexive contraction of the muscles around the anus, and this prevents the fissure from healing. As defecation is postponed due to fear of pain, the stool becomes harder and the fissure becomes deeper.
Breasts may appear around the anal canal as a result of thickening of the surrounding skin. Although anal fissure can be seen at any age, it is more common in young and middle-aged adults. It occurs equally frequently in men and women, with no gender distinction.
Anal fissures are defined in two ways: acute and chronic. There is no difference in the findings between acute and chronic fissures. Fissures that do not heal within 15-20 days, whose wound edges have become fibrotic and whose base has ulcerated are considered chronic fissures.
The location of anal fissures in the anal canal is at 12 o'clock (towards the coccyx) in 99% of men, and at 6 o'clock (towards the front) in 1% of men.
In 90% of women, it is at 12 o'clock, and in 10% of cases it is at 6 o'clock. Anal fissures are rarely located on the side walls. In atypically located fissures, diseases such as inflammatory diseases of the intestine such as Crohn's, tuberculosis, syphilis, AIDS, anal abscess and anal cancers should be kept in mind in the differential diagnosis.
In the treatment of anal fissure, first of all, the patient's nutrition and toilet habits should be regulated, and then the fissure should be treated with stool softening drugs, local anesthetic creams or warm sitz baths used for muscle relaxation, and locally effective creams.
In patients who do not benefit from these treatments, muscle relaxation should be achieved with Botox application or surgery.